Treatment Of Bursitis Of The Foot
Bursitis is an inflammation of a bursa. The heel has three areas that are involved in bursitis. Retrocalcaneal Bursa which is located between the Achilles tendon and heel bone. Subcutaneous calcaneal bursa which is located between the skin and where the Achilles tendon attaches to the heel bone. Plantar-calcaneal bursitis is located between the heel bone and the plantar fascia (thick fibrous tissue that inserts into the heel bone).
Causes
Although rare, bursitis also may be caused by an infection, known as septic bursitis. This is a serious medical condition that requires antibiotics to treat the infection and prevent its spread to other points in the body or the bloodstream. Septic bursitis may cause the back of the ankle to become red or hot. The person may also get the chills or fever and may feel sick and tired. Typically this type of bursitis would be suspected if there has been any history of an open wound in the area, such as a blister.
Symptoms
Symptoms include pain at the back of the heel, especially when running uphill or on soft surfaces. There will be tenderness and swelling at the back of the heel which may make it difficult to wear certain shoes. When pressing in with the fingers both sides are the back of the heel a spongy resistance may be felt.
Diagnosis
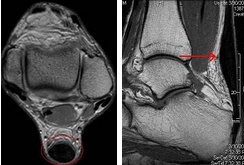
Careful examination by your physician or physiotherapist can determine if the inflammation is from the Achilles tendon or from the retrocalcaneal bursa. Tenderness due to insertional Achilles tendinitis is normally located slightly more distal where the tendon inserts into the back of the heel, whereas tenderness caused by the retrocalcaneal bursa is normally palpable at the sides of the distal Achilles tendon. Diagnosis can be confirmed with an ultrasound investigation, MRI or CT scan.
Non Surgical Treatment
Gradual and progressive stretching of the Achilles tendon. Exercises to strengthen and support the ankle. Rest or reduced weight bearing activities. Immobilisation in a cast for 4-6 weeks for severe cases. Ice. Proper fitting and supportive footwear. Massage. Joint mobilisation. Anti-inflammatory medications: only if this does not have adverse results with the patient's current medication. Heel pads and heel lifts. Footwear Advice. Strapping and padding Orthoses/innersoles. The orthotics prescribed and designed by the podiatrists at the Heel and Arch Pain Clinic (affiliated with Beyond Podiatry) are made to align the foot in the correct posture. Surgery is indicated in severe cases when conservative treatment has not resolved the problem.
Surgical Treatment
Surgery is rarely done strictly for treatment of a bursitis. If any underlying cause is the reason, this may be addressed surgically. During surgery for other conditions, a bursa may be seen and removed surgically.
Non Surgical Hammertoe Treatment
 Overview
Overview
A Hammer toe can be flexible or rigid. Hammertoes often start out flexible and become rigid over time as your toe becomes accustomed to its crooked position. Flexible hammertoes are less serious than rigid hammertoes, as they can be easily diagnosed and treated in their initial stages. Flexible hammertoes are named as such because your affected toe still possesses some degree of movement.
Causes
Hammer toe may also be caused by other medical conditions such as rheumatoid arthritis, osteoarthritis, or stroke because these forms of illnesses involve affectation of the person's muscles and nerves. Diabetes is also a causative factor for hammer toes due to diabetic neuropathy, which often times accompanies advanced instances of diabetes. Injury to a person's toes may also cause hammer toes, particularly if the injury involves breaking of the toes. In some instances, hammer toes may be hereditary. Some people may be genetically predisposed to develop the condition because of the natural structure of their bodies.
 Symptoms
Symptoms
Common reasons patients seek treatment for toe problems are toe pain on the knuckle. Thick toe calluses. Interference with walking/activities. Difficulty fitting shoes. Worsening toe deformity. Pain at the ball of the foot. Unsightly appearance. Toe deformities (contractures) come in varying degrees of severity, from slight to severe. The can be present in conjunction with a bunion, and develop onto a severe disfiguring foot deformity. Advanced cases, the toe can dislocate on top of the foot. Depending on your overall health, symptoms and severity of the hammer toe, the condition may be treated conservatively and/or with surgery.
Diagnosis
Your healthcare provider will examine your foot, checking for redness, swelling, corns, and calluses. Your provider will also measure the flexibility of your toes and test how much feeling you have in your toes. You may have blood tests to check for arthritis, diabetes, and infection.
Non Surgical Treatment
What will a doctor do? Treat any foot complaints such as corns, calluses by periodically reducing the lesion and applying appropriate pads and dressings. Recommend the silicone toe prop. If an infection is present, then anti-septic dressings, antibiotics and pads to redistribute pressure away from the lesion may be necessary. In the case of a mallet toe, trigger toe or claw toe. If a corn occurs at the end of the toe, a silicone or leather hammertoe prop may be used to straighten the toe. In a hammertoe deformity, a silicone prop to redistribute pressure away from a corn may be necessary. The doctor may give footwear advice. In severe cases, corrective surgery may be necessary. The doctor may recommend orthosis to correct a mechanical complaint of the foot, such as 3/4 length silicone insoles.
Surgical Treatment
Surgical correction is necessary in more severe cases and may consist of removing a bone spur (exostectomy) removing the enlarged bone and straightening the toe (arthroplasty), sometimes with internal fixation using a pin to realign the toe; shortening a long metatarsal bone (osteotomy) fusing the toe joint and then straightening the toe (arthrodesis) or simple tendon lengthening and capsule release in milder, flexible hammertoes (tenotomy and capsulotomy). The procedure chosen depends in part on how flexible the hammertoe is.
Bunions Reasons Signs And Symptoms And Treatment Options
Overview
 A bunion is a bony prominence on the side of the foot, at the base of the big toe joint. This enlargement of the joint, spurring, bump or lump can be aggravated by sports and tight shoes. There is progressive movement of the big toe outward, toward the other toes. As the ?bump? gets bigger, shoes can increase pressure on the base of the big toe causing more and more discomfort or pain. The term Hallux Valgus is the medical name for this condition.
A bunion is a bony prominence on the side of the foot, at the base of the big toe joint. This enlargement of the joint, spurring, bump or lump can be aggravated by sports and tight shoes. There is progressive movement of the big toe outward, toward the other toes. As the ?bump? gets bigger, shoes can increase pressure on the base of the big toe causing more and more discomfort or pain. The term Hallux Valgus is the medical name for this condition.
Causes
People born with abnormal bones (congenital) in their feet. Inherited foot type. Foot injuries. Inflammatory or degenerative arthritis causing the protective cartilage that covers your big toe joint to deteriorate. Wearing high heels forces your toes into the front of your shoes, often crowding your toes. Wearing shoes that are too tight, too narrow or too pointed are more susceptible to bunions. Pain from arthritis may change the way you walk, making you more susceptible to bunions. Occupation that puts extra stress on your feet or job that requires you to wear ill-fitting shoes. The tendency to develop bunions may be present because of an inherited structural foot defect.
Symptoms
Symptoms often include pain, swelling, and abnormal position of the first toe. The technical term for bunions is ?hallux valgus? (HV). This refers to the first toe or hallux moving away or abducting from the middle of the foot and then twisting in such a way that the inside edge actually touches the ground and the outside edge turns upward. This term describes the deviation of the toe toward the outside part of the foot. If left untreated, bunions can worsen over time and cause considerable difficulty in walking, discomfort, and skin problems such as corns. In some cases, a small bursa (fluid-filled sac) near the joint becomes inflamed. This condition is known as bursitis and can cause additional redness, swelling, and pain. Less frequently, bunions occur at the base of the fifth toe. When this occurs, it is called a ?tailor?s bunion? or bunionette.
Diagnosis
People with bunions may be concerned about the changing appearance of their feet, but it is usually the pain caused by the condition that leads them to consult their doctor. The doctor will evaluate any symptoms experienced and examine the affected foot for joint enlargement, tissue swelling and/or tenderness. They will also assess any risk factors for the condition and will ask about family history. An x-ray of the foot is usually recommended so that the alignment of big toe joint can be assessed. This would also allow any other conditions that may be affecting the joint, such as arthritis, to be seen.
Non Surgical Treatment
When a bunion first begins to develop, take good care of your feet. Wear wide-toed shoes. This can often solve the problem and prevent you from needing more treatment. Wear felt or foam pads on your foot to protect the bunion, or devices called spacers to separate the first and second toes. These are available at drugstores. Try cutting a hole in a pair of old, comfortable shoes to wear around the house. 
Surgical Treatment
Most bunions can be treated without surgery. But when nonsurgical treatments are not enough, surgery can relieve your pain, correct any related foot deformity, and help you resume your normal activities. An orthopaedic surgeon can help you decide if surgery is the best option for you. Whether you?ve just begun exploring treatment for bunions or have already decided with your orthopaedic surgeon to have surgery, this booklet will help you understand more about this valuable procedure.
Prevention
Because bunions develop slowly, taking care of your feet during childhood and early adulthood can pay off later in life. Keep track of the shape of your feet as they develop over time, especially if foot problems run in your family. Exercising your feet can strengthen them. Learn to pick up small objects, like a pencil or pebble, with your toes. Wear shoes that fit properly and don't cramp or pinch your toes. Women should avoid shoes with very high heels or pointed toes.
What Causes Overpronation Of The Feet
Over-pronation is very common and affects millions of people. To better understand this condition, we'll take a closer look at the 3 most common foot types. An estimated 70% of the population has fallen arches (or a low arch). Only 20% has a normal arch. And 10% have abnormal feet, in other words they either have flat feet or the opposite a high arched foot.

Causes
There are many biomechanical issues that can contribute to excessive pronation, including weak foot intrinsic muscles, limited ankle dorsiflexion mobility and calf flexibility, weak ankle invertor muscles (e.g. posterior tibialis), weak forefoot evertor muscles (peroneus longus), poor hip strength and control, Anterior pelvic tilting, heel InversionIn a person who overpronates, the heel bone goes into an everted position meaning that it turns out away from the midline of the body. The opposite motion of eversion is inversion. Inversion is a motion that needs to be controlled to prevent the foot from excessively pronating.
Symptoms
When standing, your heels lean inward. When standing, one or both of your knee caps turn inward. Conditions such as a flat feet or bunions may occur. You develop knee pain when you are active or involved in athletics. The knee pain slowly goes away when you rest. You abnormally wear out the soles and heels of your shoes very quickly.
Diagnosis
To easily get an idea of whether a person overpronates, look at the position and condition of certain structures in the feet and ankles when he/she stands still. When performing weight-bearing activities like walking or running, muscles and other soft tissue structures work to control gravity's effect and ground reaction forces to the joints. If the muscles of the leg, pelvis, and feet are working correctly, then the joints in these areas such as the knees, hips, and ankles will experience less stress. However, if the muscles and other soft tissues are not working efficiently, then structural changes and clues in the feet are visible and indicate habitual overpronation.

Non Surgical Treatment
If a young child is diagnosed with overpronation braces and custom orthotics can be, conjunction with strengthening and stretching exercises, to realign the bones of the foot. These treatments may have to continue until the child has stopped growing, and orthotics may need to be worn for life in order to prevent the foot reverting to an overpronated state. Wearing shoes that properly support the foot, particularly the arch, is one of the most effective treatments for overpronation. Custom-made orthotic inserts can also be very beneficial. They too support the arch and distribute body weight correctly throughout the foot. Motion-control shoes that prohibit pronation can be worn, so may be useful for those with severe overpronation. One good treatment is to walk barefoot as often as possible. Not relying on shoes to support the arch will encourage proper muscle use. Practicing yoga can help to correct poor posture and teach you how to stand with your weight balanced evenly across the whole foot.
Surgical Treatment
Calcaneal "Slide" (Sliding Calcaneal Osteotomy) A wedge is cut into the heel bone (calcaneus) and a fixation device (screws, plate) is used to hold the bone in its new position. This is an aggressive option with a prolonged period of non-weightbearing, long recovery times and many potential complications. However, it can and has provided for successful patient outcomes.
Tips On How To Spot Severs Disease?
As children reach their growth spurt in early puberty, the heel is one of the first body parts to grow to full size. Because children's bones are growing so fast, the muscles or tendons can't keep up and often become tight. The tight heel tendons can put a lot of stress on the heel, especially if a child is involved in athletics or other weight-bearing activity. Over time, too much pressure on the heel can injure it and result in Sever's disease, also called calcaneal apophysitis.
Causes
Overuse and stress on the heel bone through participation in sports is a major cause of calcaneal apophysitis. The heel?s growth plate is sensitive to repeated running and pounding on hard surfaces, resulting in muscle strain and inflamed tissue. For this reason, children and adolescents involved in soccer, track, or basketball are especially vulnerable. Other potential causes of calcaneal apophysitis include obesity, a tight Achilles tendon, and biomechanical problems such as flatfoot or a high-arched foot.
Symptoms
As a parent, you may notice your child limping while walking or running awkwardly. If you ask them to rise onto their tip toes, their heel pain usually increases. Heel pain can be felt in one or both heels in Sever's disease.
Diagnosis
Low-grade inflammation of the calcaneal apophysis cannot be seen on x-ray. Therefore, although x-rays are often done to rule out bony injuries in children with Sever's disease these x-rays are usually normal. Advanced Sever's disease can be seen on x-ray but usually the problem is treated before it reaches this point. Other diagnostic tests, such as bone scans or MRI's, are not usually required in typical cases of Sever's disease. These, or other tests, may be required to rule out other conditions, such as stress fractures of the calcaneus or other bony abnormalities that can mimic Severs disease.
Non Surgical Treatment
The treatment of Sever's disease depends upon the severity of symptoms experienced by the patient. Care is initiated with a simple program of stretching and heel elevation to weaken the force applied to the calcaneus by the Achilles tendon. If stretches and heel elevation are unsuccessful in controlling the symptoms of Sever's disease, children should be removed from sports and placed on restricted activities. Mild Symptoms. Wear a 3/8 heel lift at all times (not just during physical activity). It is important to use a firm lift and not a soft heel pad. Calf stretches 6/day for 60 seconds each. Calf stretches are best accomplished by standing with the toes on the edge of a stretching block. Moderate Symptoms. Follow the directions for minor symptoms and decrease activity including elimination of any athletic activity. In addition to stretching by day, a night stretching splint can be worn while sleeping. Severe Symptoms. Follow the directions for mild and moderate symptoms. Children should be removed from sports activities such as football, basketball, soccer or gym class. A below knee walking cast with a heel lift or in severe cases, non-weight bearing fiberglass cast, may be indicated for 4-6 weeks. The cast should be applied in a mildly plantar flexed position. Cam Walkers should not be used for Sever's Disease unless they have a built in heel lift.
Surgical Treatment
The surgeon may select one or more of the following options to treat calcaneal apophysitis. Reduce activity. The child needs to reduce or stop any activity that causes pain. Support the heel. Temporary shoe inserts or custom orthotic devices may provide support for the heel. Medications. Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, help reduce the pain and inflammation. Physical therapy. Stretching or physical therapy modalities are sometimes used to promote healing of the inflamed issue. Immobilization. In some severe cases of pediatric heel pain, a cast may be used to promote healing while keeping the foot and ankle totally immobile. Often heel pain in children returns after it has been treated because the heel bone is still growing. Recurrence of heel pain may be a sign of calcaneal apophysitis, or it may indicate a different problem. If your child has a repeat bout of heel pain, be sure to make an appointment with your foot and ankle surgeon.
Achilles Tendon Rupture Fallacies
Overview
 The largest tendon in the body, the Achilles tendon is a cord connecting the calf muscles to the heel bone. Also called the ?cord of Achilles,? the tendon gets its name from the hero of Greek myth. According to legend, Achilles was invulnerable everywhere but his heel, where a poisoned arrow eventually felled him. Because the blood supply to the Achilles tendon lessens with age, the tendon becomes vulnerable to inflammation and rupture, a fact which makes it a true ?Achilles heel? for many older patients. Achilles tendon injuries are also common among athletes and those who engage in more physically demanding activity.
The largest tendon in the body, the Achilles tendon is a cord connecting the calf muscles to the heel bone. Also called the ?cord of Achilles,? the tendon gets its name from the hero of Greek myth. According to legend, Achilles was invulnerable everywhere but his heel, where a poisoned arrow eventually felled him. Because the blood supply to the Achilles tendon lessens with age, the tendon becomes vulnerable to inflammation and rupture, a fact which makes it a true ?Achilles heel? for many older patients. Achilles tendon injuries are also common among athletes and those who engage in more physically demanding activity.
Causes
Achilles tendon rupture occurs in people that engage in strenuous activity, who are usually sedentary and have weakened tendons, or in people who have had previous chronic injury to their Achilles tendons. Previous injury to the tendon can be caused by overuse, improper stretching habits, worn-out or improperly fitting shoes, or poor biomechanics (flat-feet). The risk of tendon rupture is also increased with the use of quinolone antibiotics (e.g. ciprofloxacin, Levaquin).
Symptoms
Patients with an Achilles tendon rupture will often complain of a sudden snap in the back of the leg. The pain is often intense. With a complete rupture, the individual will only be ambulate with a limp. Most people will not be able to climb stairs, run, or stand on their toes. Swelling around the calf may occur. Patients may often have had a sudden increase in exercise or intensity of activity. Some patients may have had recent corticosteroid injections or use of fluoroquinolone antibiotics. Some athletes may have had a prior injury to the tendon.
Diagnosis
Diagnosis is made by clinical history; typically people say it feels like being kicked or shot behind the ankle. Upon examination a gap may be felt just above the heel unless swelling has filled the gap and the Simmonds' test (aka Thompson test) will be positive; squeezing the calf muscles of the affected side while the patient lies prone, face down, with his feet hanging loose results in no movement (no passive plantarflexion) of the foot, while movement is expected with an intact Achilles tendon and should be observable upon manipulation of the uninvolved calf. Walking will usually be severely impaired, as the patient will be unable to step off the ground using the injured leg. The patient will also be unable to stand up on the toes of that leg, and pointing the foot downward (plantarflexion) will be impaired. Pain may be severe, and swelling is common. Sometimes an ultrasound scan may be required to clarify or confirm the diagnosis. MRI can also be used to confirm the diagnosis.
Non Surgical Treatment
Once a diagnosis of Achilles tendon rupture has been confirmed, a referral to an orthopaedic specialist for treatment will be recommended. Treatment for an Achilles tendon rupture aims to facilitate the torn ends of the tendon healing back together again. Treatment may be non-surgical (conservative) or surgical. Factors such as the site and extent of the rupture, the time since the rupture occurred and the preferences of the specialist and patient will be considered when deciding which treatment will be undertaken. Some cases of rupture that have not responded well to non-surgical treatment may require surgery at a later stage. The doctor will immobilise the ankle in a cast or a special hinged splint (known as a ?moon boot?) with the foot in a toes-pointed position. The cast or splint will stay in place for 6 - 8 weeks. The cast will be checked and may be changed during this time. 
Surgical Treatment
Surgery offers important potential benefits. Besides decreasing the likelihood of re-rupturing the Achilles tendon, surgery often increases the patient?s push-off strength and improves muscle function and movement of the ankle. Various surgical techniques are available to repair the rupture. The surgeon will select the procedure best suited to the patient. Following surgery, the foot and ankle are initially immobilized in a cast or walking boot. The surgeon will determine when the patient can begin weightbearing. Complications such as incision-healing difficulties, re-rupture of the tendon, or nerve pain can arise after surgery. Whether an Achilles tendon rupture is treated surgically or non-surgically, physical therapy is an important component of the healing process. Physical therapy involves exercises that strengthen the muscles and improve the range of motion of the foot and ankle.
Leg Length Discrepancy Chiropractic Treatment
Leg length discrepancy is the difference in lengths of an individual?s legs. This difference may be anatomical or may be due to scoliosis, trauma/injury, arthritis, overpronation (collapse) of one foot, bowing of one leg or unequal bowing, surgery (hip or knee replacement), pelvic tilting or ageing. The difference can also be functional caused by differing forces of the soft tissues, such as weakness in muscle tissue on one side, or a weakness/tightness in joint tissue. A difference in leg lengths also results when running on indoor banked tracks, beaches and banked streets and side walks (for drainage). Many people have a measurable difference in their leg lengths which is compensated for by their bodies. As we age this compensation does not work as well. An x-ray and physical measurements will define the discrepancy and the adjustment needed.

Causes
LLDs are very common. Sometimes the cause isn?t known. But the known causes of LLD in children include, injury or infection that slows growth of one leg bone. Injury to the growth plate (a soft part of a long bone that allows the bone to grow). Growth plate injury can slow bone growth in that leg. Fracture to a leg bone that causes overgrowth of the bone as it heals. A congenital (present at birth) problem (one whole side of the child?s body may be larger than the other side). Conditions that affect muscles and nerves, such as polio.
Symptoms
The most common symptom of all forms of LLD is chronic backache. In structural LLD the sufferer may also experience arthritis within the knee and hip are, flank pain, plantar fasciitis and metatarsalgia all on the side that is longer. Functional LLD sufferers will see similar conditions on the shorter side.
Diagnosis
Leg length discrepancy may be diagnosed during infancy or later in childhood, depending on the cause. Conditions such as hemihypertrophy or hemiatrophy are often diagnosed following standard newborn or infant examinations by a pediatrician, or anatomical asymmetries may be noticed by a child's parents. For young children with hemihypertophy as the cause of their LLD, it is important that they receive an abdominal ultrasound of the kidneys to insure that Wilm's tumor, which can lead to hypertrophy in the leg on the same side, is not present. In older children, LLD is frequently first suspected due to the emergence of a progressive limp, warranting a referral to a pediatric orthopaedic surgeon. The standard workup for LLD is a thorough physical examination, including a series of measurements of the different portions of the lower extremities with the child in various positions, such as sitting and standing. The orthopaedic surgeon will observe the child while walking and performing other simple movements or tasks, such as stepping onto a block. In addition, a number of x-rays of the legs will be taken, so as to make a definitive diagnosis and to assist with identification of the possible etiology (cause) of LLD. Orthopaedic surgeons will compare x-rays of the two legs to the child's age, so as to assess his/her skeletal age and to obtain a baseline for the possibility of excessive growth rate as a cause. A growth chart, which compares leg length to skeletal age, is a simple but essential tool used over time to track the progress of the condition, both before and after treatment. Occasionally, a CT scan or MRI is required to further investigate suspected causes or to get more sophisticated radiological pictures of bone or soft tissue.
Non Surgical Treatment
Treatment depends on the amount and cause of the leg length discrepancy as well as the age of your child. Typically, if the difference is less than 2 cm we don?t recommend immediate treatment. We may recommend that your child wear a heel lift in one shoe to make walking and running more comfortable. If the leg length discrepancy is more significant, your doctor may recommend surgery to shorten or lengthen a leg. The procedure used most often to shorten a leg is called epiphysiodesis.

Surgical Treatment
Large leg length inequalities can be treated by staged lengthenings or by simultaneous ipsilateral femoral and tibial lengthenings. Additionally, lengthenings can be combined with appropriately timed epiphysiodesis in an effort to produce leg length equality. Staged lengthenings are often used for congenital deficiencies such as fibular hemimelia, in which 15 cm or more may be needed to produce leg length equality. We typically plan for the final lengthening to be completed by age 13 or 14 years, and allow at least 3 years between lengthenings. Lengthening of both the tibia and femur simultaneously requires aggressive therapy and treatment of soft tissue contractures. Curran et al[57] reported the need for surgical release of soft tissue contractures in 3 of 8 patients treated with simultaneous ipsilateral femoral and tibial lengthenings. Lengthening over an IM nail can be done in an effort to decrease the amount of time the fixator needs to be worn and to prevent angular malalignment. This technique requires that the patient be skeletally mature and it carries a higher risk of osteomyelitis (up to 15%). Additionally, if premature consolidation occurs, a repeat corticotomy is more difficult.